HIP REPLACEMENT SURGERY
Arthritis of the hip afflicts millions of patients, affecting their daily function and ability to live life without pain and activity limitation. Common symptoms of an arthritic hip include groin pain (commonly mistaken for a “pulled groin” muscle) with or without associated pain in the front of the leg sometimes down to the knee. Less frequently it is felt in the buttocks, but most often it creates discomfort with walking, sleeping, decreased rotation and flexion of the leg and the inability to perform common activities of daily living.
Treatment options include Non-Steroidal Anti-Inflammatories (NSAID’S such as Ibuprofen, Naproxen, Celebrex, Meloxicam and others), physical therapy as well as activity modification. Injections of cortisone are occasionally helpful but generally not as beneficial in the hip joint as other joints such as the knee and shoulder.
When the symptoms are causing the patient to “look at life from the sidelines”, the option of hip replacement becomes an excellent treatment option.
WHAT TO EXPECT
DURING THE HOSPITAL STAY
Abrazo Scottsdale Hospital has been transformed into a surgical and orthopedic hospital that is dedicated to providing excellent care to its patients. The staff and administration are committed to making this hospital the premier site in Phoenix for patients to undergo joint replacement surgery using the most current and innovative technologies available.
A pre-op “joint class” is offered to patients so they can learn more about what to expect during their hospital stay. It is also encouraged to be seen in the Pre-Admission Testing unit before surgery when possible so that the health and anesthesia needs can be fully ascertained before the day of surgery. For those patients traveling from out of town for their surgery, alternative arrangements can be made to accommodate everyone’s needs.
The day of surgery involves checking in, a nursing evaluation, starting and IV in your arm and confirming the side and nature of the procedure being performed. The procedure typically takes 45 minutes from start to finish and is followed by a short stay in the recovery room. Dr Cohen uses an IV based General Anesthetic (different to most anesthetics that you might have had in the past). The technique uses five different medications administered through the vein rather than breathed in through the lungs. This combination provides pre-emptive pain relief, decreased nausea, easier time “waking up” and improved pain control after the surgery. Local anesthetic is also injected around the surgical site during the procedure to reduce post-op pain. This allows mobilization out of bed very soon after surgery once you have arrived on the Orthopedic Unit. Physical Therapy will see you and assist you in getting up and walking around the ward. This helps reduce down-time, blood clots and other issues that arise from lying in bed longer than necessary.
Oral pain medication is prescribed but patients frequently note that they used very few if any pain pills. Aspirin is started for blood clot prevention and is taken twice a day for a month (higher risk patient might be placed on different medications when deemed appropriate by the surgeon/medical team). An anti-inflammatory medication is prescribed as well for approximately one month to assist in healing and pain management. A walker is used briefly followed by a cane (most transition to independent walking within 2 weeks, unless otherwise prescribed or recommended), and is primarily used for balance while gaining confidence with the new hip.
Outpatient physical therapy can be utilized following discharge but ultimately, the best therapy for hip replacement is to walk and perform gentle motion exercises which will be reviewed by the hospital therapist.
Most patients spend no more than one night in the hospital and in many instances, patients go home the day of surgery.
WHAT TO EXPECT
AFTER THE HOSPITAL
Following discharge from the hospital, it’s important to have some help for the first few days to assist with driving, cooking, getting comfortable after surgery or whatever other issues might arise. It is rarely necessary to go to a transitional care facility unless the social situation requires this, in which case the hospital will make arrangements during your stay.
It is recommended that you may drive when YOU feel safe to drive. You should be off all pain medication, feel like the leg is under your full control to operate a motor vehicle and that it’s safe for you to do. It is not up to the surgeon or therapist to give you an exact time frame when you can drive. Please discuss with Dr. Cohen if further suggestions are necessary.
You may progress as you see fit for the first six weeks. Since there are no positional restrictions imposed on the hip, a regular chair and toilet seat are acceptable. The wound does not require any additional care other than removing the bandage that is placed in surgery, typically 5-7 days post op. You may apply wound healing remedies such as Vitamin E or Maderma if desired after 2 weeks. Showering can begin 3 days post op with the bandage in place. No submerging in a pool or tub for 14 days. The wound is closed with dissolvable sutures and nothing needs to be removed from the wound.
It is suggested that only low impact activities are performed the first 6 weeks. The bone takes around 4-6 weeks to fully adhere to the implants placed during surgery. Any high impact forces might disrupt this process and impede the desired long-term adherence of bone to the metal interface. Walking, swimming, upper body gym exercises, stationary bike, elliptical trainer, chipping and putting at the golf range are all perfectly fine as long as you feel comfortable doing so. Any additional questions regarding specific activities can be directed to Dr. Cohen’s team for clarification.
The first post-op appointment is 6 weeks after surgery. This may seem like a long time, but in an effort to streamline this entire process for you, Dr. Cohen does not need to make you return sooner while you are recovering. However, if at any time there are questions or concerns, you are encouraged to call the office and request an appointment. Every effort will be made to see you promptly, either by Dr. Cohen or his Physician Assistant. X-Rays will be taken at the office and an exam performed to ensure that the hip has healed well and the implants have remained in their original position. An opportunity to ask questions and plan for future activities will be available, as well to ensure that you are comfortable, satisfied and are able to return to your life without pain and restriction!
KNEE ARTHRITIS
AND JOINT REPLACEMENT
Knee Arthritis
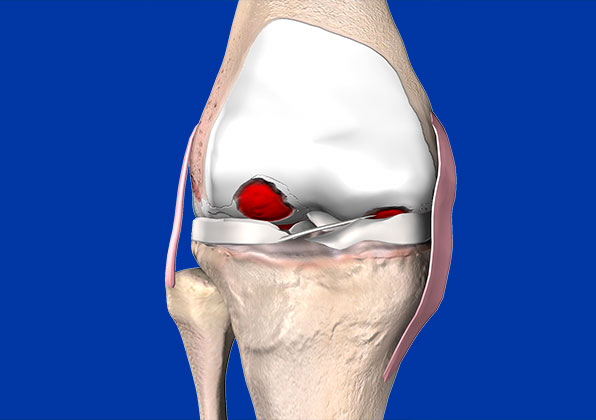
Arthritis of the knee afflicts millions of people around the world and is a major source of disability. Causes include osteoarthritis which is a “wear and tear” disease of the natural cartilage that lines the ends of our bones. Other causes include inflammatory arthritis such as Rheumatoid Disease and Psoriatic Arthritis, Post Traumatic Arthritis and several other less common causes.
Symptoms include
• pain
• swelling
• decreased range of motion
• catching or grinding associated with pain
• instability of the joint
• decreased ability to walk without pain
• pain going up or down stairs and inclines
• night pain
Early interventions might include:
- NSAID’s (non-steroidal anti-inflammatory medications such as Ibuprofen, Naprosyn, Celebrex, Meloxican and Diclofenac) if not medically contra-indicated.
- Activity modification along with ice/heat and rest also help to alleviate symptoms associated with joint pain.
- A Cortisone injection might be appropriate for some patients and can provide good relief, in some instances for months or more at a time.
- Visco-supplementation is purified joint fluid that is appropriate in early stages of the disease and usually comes in a series of 3 or 5 injections performed a week apart. These might provide relief in some patients for extended periods of time and can be performed every 6 months.
- Stem cell therapy has recently gained popularity, however it has not been proven to improve symptoms or alter the disease process as it relates to arthritis of the knee joint. It is also not a covered benefit by insurance and is a fee for service procedure. It can be used and has more favorable indications for soft tissue ailments such as Tendonitis and other muscle injures. Dr. Cohen does not currently advocate the use of these injections for arthritis of the hip or knee.
- Physical therapy might be prescribed to help improve joint movement and stability to optimize the knee function and reduce pain.
Joint Replacement options:
As the disease progresses to a point where there is minimal to no cartilage left and the bones are rubbing on each other, pain increases, function decreases, and the conservative options become less effective. It is at this point that a patient usually seeks the advice of an Orthopedic Surgeon who performs joint replacement surgery. It will be up to the surgeon to decided what specific procedure is indicated and ultimately the patient’s decision whether or not to proceed.
MAKO Partial Knee Replacement
Dr Cohen performs single compartment replacement surgery when it affects the medial (inner) compartment and patellofemoral joint. This is less frequently performed than full knee replacement but is a great option if indicated.
Advantages include:
-Smaller surgical approach
-Reduced recovery time
-Preservation of the two healthy compartments not affected by the wear of cartilage
-Outpatient surgery
Disadvantages include:
-Small potential for other parts of the knee to become arthritic
-Conversion to a full knee replacement in the future if the disease progresses (unlikely but possible)
-Not everyone is a candidate
MAKE TOTAL KNEE REPLACEMENT
Dr Cohen performs almost all his knee replacements using MAKO Robotic technology to achieve a customized placement of the implants that helps reduce pain, decrease rehabilitation time and more comfortably fits the soft tissue envelope for each individual patient. There are numerous publications that support the benefits and claims of robotic knee replacement, as well as patient testimonials to support these claims.
How is it different than regular knee replacement? A CT scan is performed prior to surgery in order to create a customized 3D model of the patient’s diseased knee. This highly accurate model allows the team to make a very detailed plan for the procedure prior to the operation. The surgeon now has a greater appreciation for the subtle nuances that every patient brings into the operating room.
During the surgical procedure, pins are placed in the bone in order to establish communication with the robotic system. Your joint anatomy is then “registered” in real time and space to the CT scan model, and confirmed to a tolerance of no more than 0.5mm. This level of accuracy allows the system to be extremely accurate in finalizing the plan and execution of the plan.
The surgeon then places the knee through specific movements and tensioning of the ligaments which establishes the best plan to remove only as much bone as will be replaced by the metal and plastic components, and allow micro-adjustment of the alignment in several planes. It is this process that differentiates MAKO technology along with the final step of executing the plan by a haptically controlled robotic arm, preventing any deviation from the patient specific plan. This controlled system also greatly reduces the chance of injuring adjacent tissue by controlling the boundaries of the saw blade.
What to Expect Prior to and the day of surgery
Once the decision for surgery has been made, Dr Cohen’s dedicated team of assistants will carefully guide you through the pre-operative phase. This usually includes:
• Blood work
• EKG
• Urinalysis
• One or two PT visits to evaluate and initiate pre-surgery exercises that will help with the recovery
• CT scan for the MAKO plan
• Medical or Cardiac Clearance from your provider if indicated
• “Joint Camp” if able to attend
• Pre-Anesthesia testing at the hospital (when feasible)
The day of surgery will begin with hospital check-in, evaluation and preparation by nursing with confirmation and review of a surgical consent. An IV will be started and medications will be given as part of a pre-emptive pain management protocol. Anesthesia will perform a nerve block to reduce post-operative pain and will discuss anesthesia protocols. Dr Cohen has been using an IV based general anesthetic that has many advantages and has been very well received by his patients. It helps with post-op nausea, pain, drowsiness and provides a sense of improved clarity after the surgery. It eliminates the need for spinal anesthesia and eliminates the need for a urinary catheter.
Surgery to replace the knee takes less than an hour in most instances. However, the appropriate time will be taken to perform the operation safely and effectively. Dr Cohen has been performing his knee replacements through a Minimally Invasive Surgical approach for over 15 years. The quadricep muscle is not cut or divided which allows for a rapid return to control of the leg. Patients are able to lift the leg the day of surgery and generally able to wean from the walker or cane much faster by preserving the quadricep. The soft tissue dissection is also more conservative around the joint which helps reduce swelling, pain and apprehension to move the knee. The incision is meticulously closed with dissolvable sutures that do not require any special care nor need to be removed.
Physical therapy will evaluate you the day of surgery and walk you around the unit or a distance that is appropriate. Some patients who feel well enough to go home the day of surgery will be discharged after mutual agreement of progress by the patient, staff and support team. If preferred, a one-night stay is permitted and only if medical necessity dictates it, a longer than one night stay might occur.
Post op plans should include:
• Schedule first outpatient PT visit 4-5 days after surgery
• 6 week follow up appointment with Dr Cohen
• A walker will be arranged for post-op use for a time that is deemed necessary by the patient and/or therapist
-A cane is to be used after the walker is put aside
-Clear rugs and loose impediments around the house to avoid tripping
-A “joint buddy” to help with driving, meals and general needs until you are more independent
What to Expect Prior to and the day of surgery
Most patients are surprised by how well they are able to mobilize and get moving following their knee replacement. Dr Cohen encourages slow and steady progress under the supervision of a physical therapist who can monitor joint motion and walking patterns. Therapy usually is scheduled 2-3 times a week for 4- 6 weeks depending on progress. The providers will then determine the need for additional visits beyond 6 weeks. The main goal for the firs 6 weeks is to bend and straighten the knee as much as possible to optimize range of motion. This becomes more difficult to achieve the further out from surgery you get, so work hard and smart from the start! You won’t over stretch the incision, despite how it might feel. It’s imperative that you listen to your body. If you’re tired, rest!